This is online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs.This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
E.Laharika
Hall ticket no: 1701006040
CASE PRESENTATION :
A 46 year old male came with chief complaints of:
Burning micturition present since 10 days
Vomiting since 2 days ( 3 - 4 episode)
Giddiness and deviation of mouth since 1 day
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 10years back, he complained of polyuria for which he was diagnosed with Type 2 diabetes mellitus he was started on OHAs, 3years back OHAs were converted to insulin.
20 days back, he developed vomiting , containing food particles and non bilious. He also complained of deviation of mouth and giddiness 1 day
His GRBS was also recorded high , for which he was given NPH 10 IU and HAI 10 IU
No history of fever/cough/cold
No history of previous UTIs
No history of chest pains/palpitations/syncopal attacks
PAST HISTORY:
10yrs back patient complained of polyuria and was diagnosed with Type 2 DM and started on OHA( oral hypoglycemic agents).
OHAs were converted to insulin 3 years back
3 years back , he underwent cataract surgery
1 year back, he had h/o small injury on leg which gradually progressed to non healing ulcer extending upto below knee eventually ended with below knee amputation i/v/o development of wet gangrene
Delayed Wound healing present- wound healing took 2 months time to heal
Not a k/c/o HTN/Epilepsy/TB/BA/Thyroid disorder/CAD/CVD
Not on any other medication
No h/o blood transfusion
PERSONAL HISTORY:
Diet - Mixed
Appetite- normal
Sleep- Adequate
Bowel and bladder- Regular
Micturition- burning micturition present
Habits/Addiction:
Alcohol-
Not consuming alcohol since 1 yr.
Previously (1yr back) Regular consumption of alcohol, about 90mL whiskey consumed almost daily.Also 1 month on & off consumption pattern previously present
FAMILY HISTORY:
Not significant
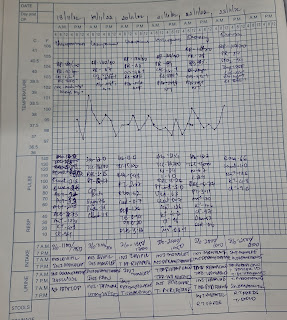
Vitals @ Admission:
BP: 110/80 mmHg
HR: 98 bpm
RR: 18 cpm
TEMP: 101F
SpO2: 98% on RA
GRBS: 124 mg/dL
GENERAL EXAMINATION:
Pallor present
No Icterus/Cyanosis/Clubbing/Koilonychia/Lymphadenopathy/Edema
No dehydration
CVS: S1S2 heard, No murmurs
RS: BAE+,NVBS
P/A: Soft, Non tender
CNS:
Patient is having altered sensorium
Reflexes: (Biceps/Triceps/Knee/Ankle/Plantar)Normal
Power: Normal(5/5) in both Upper and Lower limbs
Tone: Normal in both Upper and Lower limbs
No meningeal signs
INVESTIGATIONS:
On 19/5/22:
X ray KUB
CT scan
USG
20.05.22
LDH- 192
24hr Urinary protein- 434
24hrs Urinary creatinine- 0.5
Pus cells
21.5.22
Hemoglobin- 6.8g%
TLC- 22,500cells/cumm
Platelets- 1.4lakhs/cu.mm
Urea- 155mg/dl
Creatinine- 4.7
Uric acid- 7.1
Phosphorus- 2.0
Sodium- 126
Potassium- 2.6
Chloride- 87
22.5.22
Hemoglobin- 7.2
TLC- 17,409
Platelet count- 1.5
Urea- 162
Uric acid- 5.0
Sodium- 125
Chloride- 88
23.5.22
Hemoglobin- 6.7
TLC- 21,000
Platelet count- 1.5
Urea- 160
Uric acid- 7.5
Sodium- 130
Chloride- 97
24.5.22
Hemoglobin- 6.8
TLC- 24000
Platelet count- 1.6
Sodium- 134
Chloride- 98
27.5.22
Hb- 7
TLC- 22,000
Platelet count- 26,000
Urea- 144
Creatinine - 4.8
Uric acid-9.1
Phosphorus- 4.8
Sodium- 135
Potassium- 4.3
Chloride- 98
Fasting blood sugar- 149
29.5.22
Hb- 6.4
TLC- 14,700
Platelet count- 6000
Urea - 149
Creatinine- 4.4
Uric acid- 9.2
30.5.22
Hb- 6.4
TLC- 13,700
Platelet count- 50000
Urea - 146
Creatinine- 4.2
Uric acid- 9.1
X ray KUB
PROVISIONAL DIAGNOSIS:
Right emphysematous pyelonephiritis and left acute pyelonephiritis
Encephalopathy secondary to sepsis
TREATMENT:
Day 1 to Day 3:
INJ. MEROPENEM 500mg IV BD
INJ. ZOFER 4mg IV TID
INJ. PAN 40mg IV OD
IV Fluids- NS,RL @ 100 mL/hr
BP/HR/RR/SpO2 charting
Temp charting 4th hrly
RT feeds- 2nd hrly 100 mL water
Day 4
INJ. MEROPENEM 500mg IV BD
INJ. ZOFER 4mg IV TID
INJ. RANTAC 50mg IV OD
INJ. KCl 2 Amp in 500 mL NS over 4.5 hrs infusion
IV Fluids- NS,RL @ 100 mL/hr
SYP. POTCHLOR 10 mL in 1 glass of water TID
SYP. MUCAINE GEL 10 mL PO TID
7 point profile
BP/HR/RR/SpO2 charting
Temp charting 4th hrly
RT feeds- 2nd hrly 100 mL water
Day 5 to Day 10:
INJ. MEROPENEM 500mg IV BD (Day 6)
INJ. ZOFER 4mg IV TID
INJ. RANTAC 50mg IV OD
INJ. LASIX 40 mg IV BD
IV Fluids- NS,RL @ 100 mL/hr
SYP. MUCAINE GEL 10 mL PO TID
GRBS 7 point profile
INJ.HAI SC TID ACC to GRBS
TAB.DOLO 650 mg SOS
BP/HR/RR/SpO2 charting
Temp charting 4th hrly
Day 11:
INJ. COLISTIN 2.25 MU IV OD(Day 4)
INJ. ZOFER 4mg IV TID
INJ. RANTAC 50mg IV OD
INJ. LASIX 40 mg IV BD
IV Fluids- NS,RL @ 100 mL/hr
SYP. MUCAINE GEL 10 mL PO TID
GRBS 7 point profile
INJ.HAI SC TID ACC to GRBS
TAB.DOLO 650 mg SOS
Day 12:
SDP Transfusion done I/v/o low platelet count
Pre transfusion counts:
Hb:6.2 g/dL
TLC:14700
PLt:6000
Post transfusion counts:
Hb:6.4
TLC:13700
PLt:50000
INJ. COLISTIN 2.25 MU IV OD(Day 5)
INJ. ZOFER 4mg IV TID
INJ. RANTAC 50mg IV OD
INJ. LASIX 40 mg IV BD
IV Fluids- NS,RL @ 100 mL/hr
SYP. MUCAINE GEL 10 mL PO TID
GRBS 7 point profile
INJ.HAI SC TID ACC to GRBS
TAB.DOLO 650 mg SOS
























Comments
Post a Comment