67 year old male with COPD with right heart failure
This is online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs.This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
E.Laharika
Roll no: 29
- I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
CASE PRESENTATION :
A 67 year old male , farmer by occupation, came with chief complaints of:
Pedal edema since 6 months
SOB grade 2 since 2 months
Low back ache since 2 months
HOPI:
patient was apparently asymptomatic 2 years back then he developed shortness of breath on exertion, associated with dry cough for which he went to hospital, given medication for shortness of breath.He used to take medication (inhalers)whenever he had shortness of breath.
Bilateral pedal edema since 6 months,which was insidious in onset and gradually progressive. It is pitting time.
From the last 2 months shortness of breath which was of NYHA grade 2 progressed to grade 3 associated with PND. Patient complain of low back ache since 2 months which was insidious in onset gradually progressive .There is no radiation of pain . Pain is not relieved on medication.
Since one week pain was aggravated and patient was unable to sit or stand.
PAST HISTORY:
Pt is a k/c/o COPD and is on inhalers since 2 years
No h/o of DM , HTN, Asthma, TB
No h/o any drug allergies
PERSONAL HISTORY:
Diet- mixed
Sleep- adequate
Appetite- normal
Bowel and bladder movements- Regular
Smoking- smoked bd for about 26 years and stopped 14 years back
Occasional alcoholic- last binge 6 months back
FAMILY HISTORY: Not significant family history
GENERAL EXAMINATION:
Pt is conscious, coherent and cooperative
No pallor, no icterus, no Cyanosis, no clubbing, no lymphadenopathy
Pedal edema- present
VITALS:
Day 1
TEMPERATURE :101F
BP.:120/80mmhg
PR.:110bpm
RR.:28/min
SPO2.:88%at room air 99%@ 5litres of 02
GRBS: 133mg/dl.
Day 2
BP.:120/80mmhg
PR.:88bpm
RR.:22/min
SPO2.:98%at room air
GRBS: 150mg/dl.
DAY 3
BP.:110/70mmhg
PR.:86bpm
RR.:18/min
SPO2.: 98% at room air
GRBS: 109mg/dl.
DAY 4
BP.:120/80mmhg
PR.:110bpm
RR.:22/min
SPO2.:99% at room air
GRBS: 100mg/dl.
SYSTEMIC EXAMINATION:
Respiratory system:
Inspection:
No tracheal deviation
Chest bilaterally symmetrical
No dilated veins,pulsations,scars, sinuses.
No drooping of shoulder.
Palpation:
No tracheal deviation
Apex beat- 5th intercoastal space,medial to midclavicular line.
Tenderness over chestwall- present.
Vocal fremitus- normal on both sides
Measurements:
Anteroposterior diameter- 21cm
Transverse diameter-30cm
Ratio: AP/T- 0.7
Chest expansion: 2.5 cm
Percussion:
Supraclavicular
Infraclavicular.
Mammary
Axillary
Infraaxillary
Suprascapular
Infrascapula
Interscapular
Right side and left side- resonant in above areas.
Auscultation:
Vesicular breath sounds
Rhonchi heard.
Decreased breath sounds.
Cardiovascular system:
JVP- raised.
Auscultation:
Mitral area, tricuspid area, pulmonary area, aortic area- S1,S2 heard.
Abdominal examination:
Abdomen distended, umbilicus- inverted
Soft, tenderness present
No organomegaly.
Central nervous system:
No focal neurological deficit.
INVESTIGATIONS:
Ph-7.4
Pco2- 43.3
Po2-97.4
So2-95
Hco3-26.7
On 4 ltrs o2
BGT-A positive
RBS- 132 mg/dl
Blood urea- 50mg/dl
Hemogram:
Hb - 11 gm/dl
TLC - 12400
N/L/E/M-92/3/2/3
PCV-36.2.2
MCV-75.9.9
MCH-23.1
MCHC-30.4
RDW - CV-17.4
PLT- 2.30
NC/NC with neutrophilic leucocytosis
Phosphorous-3.6 mg/dl
Serum ca+2 - 9.2 mg/dl
Serum creatinine- 0.9
LFT:
Tb - 1.71
Db- 0.50
SGOT(AST) - 41
SGPT(ALT) - 38
ALP-250
Tp-5.4
Albumin-2.98
A/G - 1.23
SERUM ELECTROLYTES:
Na+ - 141
K+ - 4.3
Cl - - 97
Troponin 1 - negative
ECG:
X ray
Diagnosis: COPD with right heart failure
Low back pain under evaluation
TREATMENT-
1.NEBULISATION WITH IPRAVENT AND BUDECORT-8th HOURLY
2.INJ LASIX 40 MG IV/BD
CHECK BP BEFORE GIVING LASIX
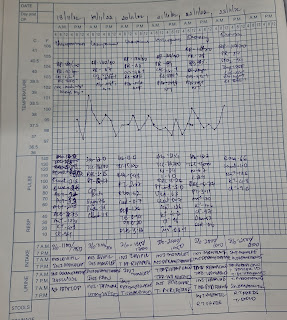
3.STRICT I/O CHARTING
4.VITALS MONITORING EVERY 4TH HOURLY
5.TAB DOLO -650 MG /PO/SOS
6.TAB HYDRALAZINE 12.5 MG PO/BD
7.TAB CARVEDILOL 3.125 MG PO
8.TAB ECOSPRIN -AV(75/20. MG) x PO/OD
















Comments
Post a Comment